While hospitals have faced a multitude of challenges since the beginning of the COVID-19 pandemic, this year is proving to be just as demanding for hospitals in Puerto Rico. Hospitals provide vital care on the Island, but the number and scale of financial, operational, systemic, and human capital challenges they face can be daunting. How can hospital administrators improve their financial position without relying on reimbursement increases? How can Operations Managers improve processes while enhancing healthcare workers’ engagement? How can these improvements result in a better patient experience?
In this insight, V2A provides an overview of the current state of hospitals on the Island and offers various approaches to address some of their longstanding issues.
Context – Industry composition and hospital density
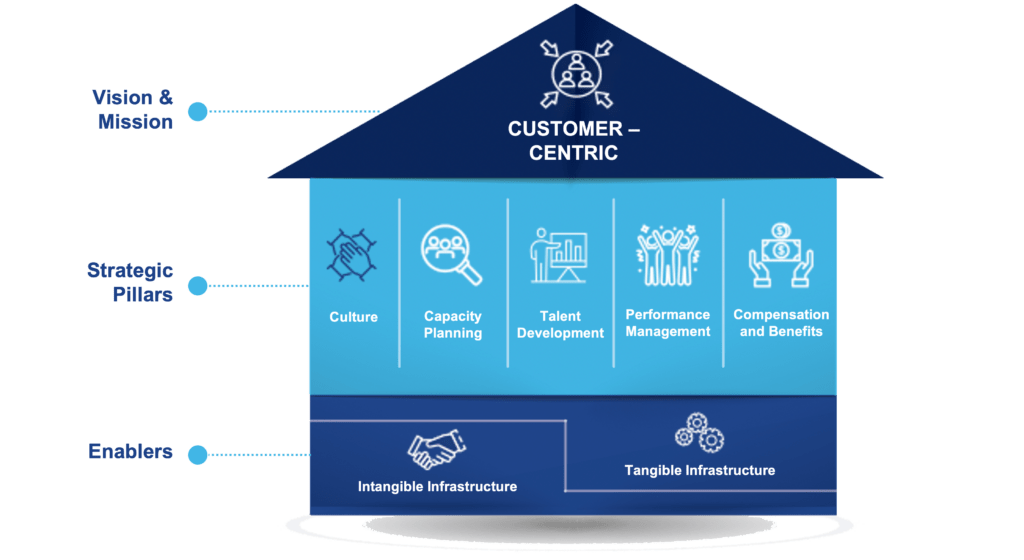
Puerto Rico has a higher hospital density than the mainland US, and also with large geographic areas without nearby hospitals. In the US, there are 1.83 hospitals for every 100k inhabitants1, whereas Puerto Rico has 2.3 hospitals per 100k inhabitants. While these numbers signal a healthy hospital density, the concentration of hospitals in the metro area and other urban areas leaves much of the island with reduced hospital access, as shown in Figure 1 below.
Figure 1: Hospital locations in Puerto Rico
There are approximately 9,350 inpatient beds with a presence in 24 of the 78 Municipalities. The Metro Pavía system is the largest hospital group with 11 hospitals and 15% of all inpatient beds throughout the Island, followed by HIMA with 5 hospitals and 13% of inpatient beds (mainly in the Metro and East regions) and Doctors Group with 4 hospitals and 7% of inpatient beds. While these groups have a notable proportion of hospitals in their portfolios, most hospitals do not belong to any group.
Financials – Longstanding issues remain
Like hospitals in the mainland, Puerto Rico hospitals face financial challenges. However, Puerto Rico faces some unique disadvantages that contribute to lower revenues.
Medicare and Medicaid programs represent 80% of the market in dollar terms. This segmentation has a widespread impact on the healthcare system and hospitals are no exception. Not only does Puerto Rico have one of the highest rates of collective Medicare and Medicaid enrollment in the country, but it also receives Medicaid reimbursement at lower levels than its mainland counterparts. As stated in our insight, “Healthcare in Puerto Rico, Challenges and Our Big Opportunity2”, even with reimbursement rate increases planned for this year, Puerto Rico will continue to lag all other jurisdictions, with a $2,142 annual expense per beneficiary, while the US average is four times higher at $8,541.
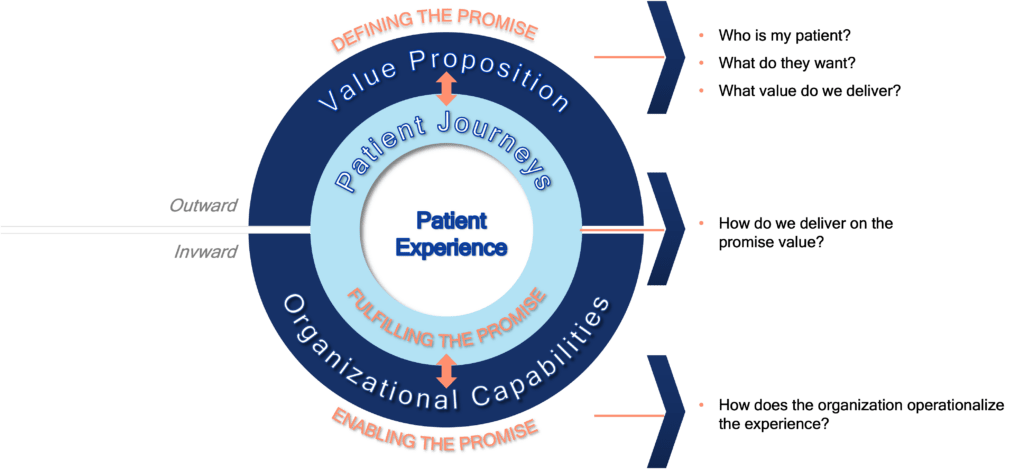
In addition to these low reimbursement rates, in recent years, hospitals have been struggling to maintain overall profitability. Thirty-five percent of the Island’s hospitals have negative operating margins3. These numbers have improved in the past five years, as shown in Figure 2, but a portion of the hospital sector remains in financial distress.
Figure 2: Hospitals with negative income margin in Puerto Rico
Globally, inflation rates have been rising, which is felt across the healthcare sector, the same as in all other sectors. Hospital expenses have increased 23% in less than a decade, with labor and supply costs driving the most dramatic budget impacts4. This, coupled with global supply chain issues, has led to severe hospital cost increases.
To ease the inflation burden on operating costs, hospital administrators should develop cost containment and revenue generation strategies. Hospitals can improve their operational efficiency by streamlining processes, reducing waste, optimizing staffing levels and implementing new technologies. They can also leverage purchasing power through fixed pricing arrangements and streamlined contract negotiations. Hospitals that belong to a hospital system can benefit from economies of scale in their purchases. Revenue stream diversification can be achieved by offering additional services or expanding their patient base. This can include opening new clinics, or preventive/wellness centers, offering new specialties, or partnering with other healthcare providers. In addition, hospitals can explore other sources of non-patient-driven revenues, such as funding in the form of federal grants or from philanthropic organizations.
People – Healthcare worker crisis
Hospitals in Puerto Rico are and will continue to be affected by a lack of personnel and skills mismatch.
All over the US, hospitals are feeling staffing stress mainly related to inflationary wage increases. In Puerto Rico, these staffing challenges are compounded by the healthcare worker crisis, in which doctors and nurses educated and trained in Puerto Rico are leaving for the mainland US to pursue higher salaries and better working conditions. Last October the PR Hospital Association asked the Governor of Puerto Rico, Pedro Pierluisi, to lobby Congress for 500 million dollars in Medicaid funding to increase compensation for hospital healthcare workers on the island.
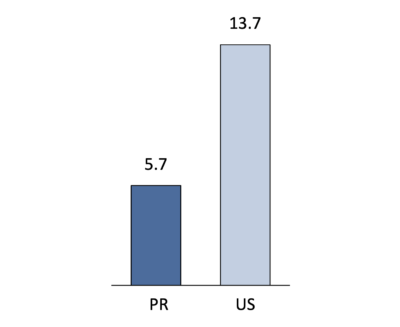
The lack of qualified professionals in a hospital setting is particularly evident in some specialties, including Emergency Medicine Physicians, as shown in Figure 3 below. Puerto Rico has 58% fewer emergency physicians per 100k than the mainland US5.
Figure 3: Emergency physicians per 100k population in PR and US
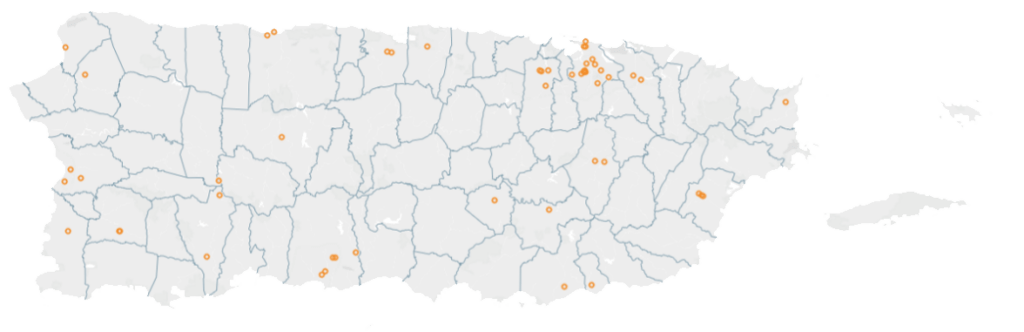
Attracting and retaining talent becomes paramount to managing hospital healthcare worker crises. High salaries alone are not sufficient to obtain good levels of workforce engagement. Hospital leaders should take into consideration other factors, such as the desired culture, capacity planning, people development, and performance management. The desired culture in a hospital setting should prioritize the needs of the patients and promote a collaborative and respectful environment where everyone is committed to delivering the best possible care. The culture should encourage collaboration among all healthcare team members, including physicians, nurses, pharmacists, and support staff. This includes sharing knowledge, ideas, and resources to improve patient outcomes. Hospitals need to plan their staffing to meet work demands proactively. Staffing means having the right people, with the right skills, at the right time, by predicting volumes and managing shifts adequately to cover peak demand. Hospital leadership should support ongoing learning and professional development for all employees. This includes providing opportunities for training, education, and skills development to enhance the quality of care provided, including critical soft skills such as being empathetic and treating patients with dignity and kindness.
All these critical elements are considered within V2A’s Human Capital framework6 (Figure 4).
Figure 4: V2A’s Human Capital Framework
Operations – The elusive promise of excellence
Hospitals in Puerto Rico are subject to the same compliance requirements derived from Federal and state regulations as US hospitals but with lower reimbursements. This contributes to gaps in quality measures.
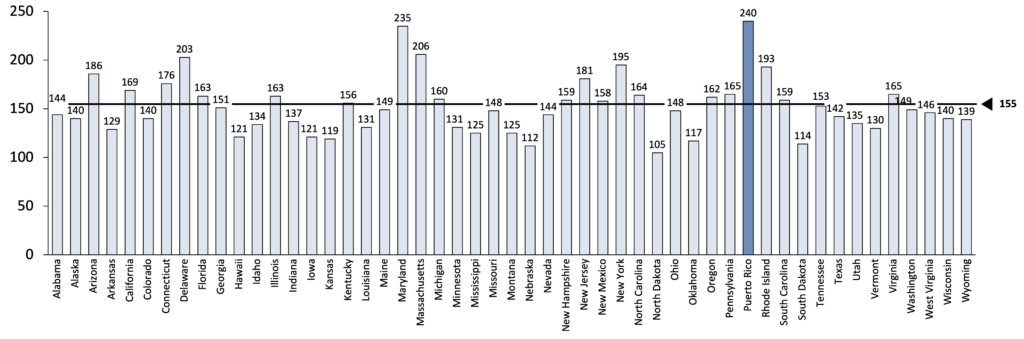
The lack of physicians in certain specialties may partly explain these gaps. Given the Emergency Department quality metrics, the lack of emergency physicians (ED) shown above is particularly concerning. As seen in Figure 5, Puerto Rico has the highest average wait time7 in the ED before being sent home, 240 minutes, compared to a US average of 155 minutes.
Figure 5: Average wait time in Emergency Department by State
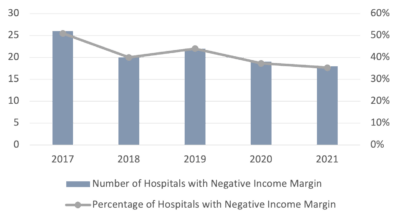
Streamlining operations can help improve the patient experience while reducing operating costs. It all starts with understanding the patient’s needs and desires and the hospital’s ability to deliver what they need. For example, in the ED, efficient and well-organized triage is critical to ensuring that patients receive timely care. Clear communication is key to reducing patient anxiety and ensuring they understand their medical condition and treatment plan. The environment should be welcoming, with comfortable seating, cleanliness, nice lighting and décor, and access to snacks, water, and other amenities. As previously discussed, patients should always be treated with respect and dignity. Finally, follow-up care is crucial to ensure readmissions are avoided.
V2A’s Patient Experience framework can help hospitals clearly define their value proposition, map the desired patient journeys and ensure the organizational capabilities are in place to deliver the desired experience.
Figure 6: V2A’s Patient Experience Framework
Systemic – Collaboration for better patient care
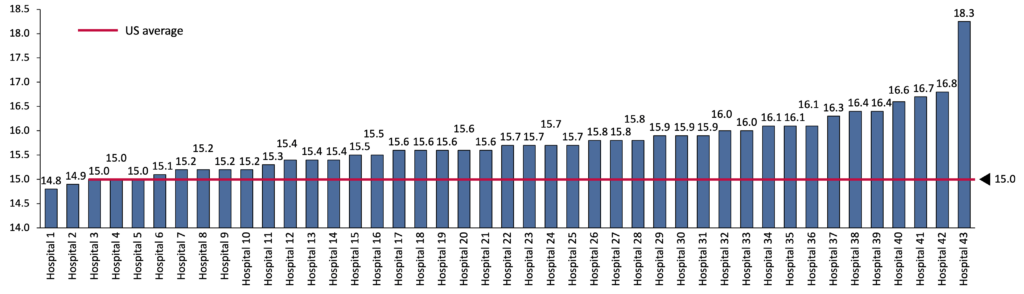
As Figure 7 shows, the readmission rates in all but two Puerto Rico hospitals8 that reported results are above the US average.
Figure 7: Readmission rates in Puerto Rico hospitals
Often, little care coordination between the government, payers, and providers yields poor patient outcomes, such as high readmission rates. There is a real need to improve collaboration and coordination between key stakeholders to ensure a seamless patient journey. Patients should be able to easily navigate from the PCP to the specialist, to the hospital and post-acute care, such as rehab or home care. It is encouraging to see the shared strategies that hospitals and primary care providers are putting in place to improve the patient journey, reduce readmissions and enhance the overall quality of care.
Conclusion
Hospitals in Puerto Rico face many challenges. Inflation will likely continue to hurt hospital margins as well as their ability to attract and retain talent. In Puerto Rico, the talent question is exacerbated by an ongoing healthcare workers crisis. As the key component of our healthcare infrastructure, hospitals can benefit from a holistic approach to managing their finances, people, and operations and collaborating with other players to serve patients better.
Sources:
[1] American Hospital Association
[2] https://v2aconsulting.com/healthcare-in-puerto-rico-challenges-and-our-big-opportunity/
[3] AHD – American Hospital Database
[4] https://revcycleintelligence.com/news/hospital-expenses-have-increased-23-in-less-than-a-decade
[5] Association of American Medical Colleges “Physician Specialty Data Report 2020” and Informe Estadístico de Médicos y Profesionales de la Salud en Puerto Rico, Departamento de Salud 2016-2018; V2A analysis
[6] https://v2aconsulting.com/radiografia-del-empleador/
[7] American Hospital Directory database from 10/1/2020 to 9/30/2021; V2A analysis
[8] American Hospital Directory database from 10/1/2018 to 6/30/2021; V2A analysis
Disclaimer
Accuracy and Currency of Information: Information throughout this “Insight” is obtained from sources which we believe are reliable, but we do not warrant or guarantee the timeliness or accuracy of this information. While the information is considered to be true and correct at the date of publication, changes in circumstances after the time of publication may impact the accuracy of the information. The information may change without notice and V2A is not in any way liable for the accuracy of any information printed and stored, or in any way interpreted and used by a user.
Here are some related insights on healthcare:
V2ATalks Healthcare: Una conversación con el Licenciado Humberto Pérez, Director Ejecutivo del Hospital Dr. Susoni
Healthcare in Puerto Rico: Challenges and Our Big Opportunity
ONLY ENGLISH VERSION