Overview
Puerto Rico’s health system continues to face longstanding funding issues, hospital financial struggles, and a shortage of healthcare workers. Although the challenge is clear and present to all who work in this industry, there is a significant opportunity to pull us away from pessimism. Fragmented as the health system is, we can improve the experience for both patients and providers. As consultants and experts in this field, we see encouraging trends that pave the way for this transformation. We propose applying rigorous methods to understand the true patient and provider experience and dive deep into each of their journeys. This way, we can redesign a new, human-centered experience that provides what patients and providers need while complying with all rules and regulations, despite the funding inequalities and the long-standing crisis of healthcare workers.
Funding: The gap persists
Medicare Advantage (MA) and Medicaid represent $8 of every 10 dollars spent on healthcare in Puerto Rico. The funding levels of these two programs determine the degree of care available for over 2 million people on the Island.
Medicaid
The Federal government has assigned $19.4 billion in Medicaid funds for the next 5 fiscal years, at a rate of $3.8 billion per year, representing a sensible increase versus previous years. The local regulator, ASES, has stated it will dedicate the funds to increase provider rates from 70% to 80% of the Medicare Fee Schedule, with some specialties even going to 100%; raise the eligibility threshold for Medicaid to 85% of the federal poverty level, up from a statutory 55% FMPA matching rate; and provide new services such as non-emergent transportation. (1)
Despite this rate increase, Puerto Rico will continue to lag all other jurisdictions, with a $2,142 annual expense per beneficiary, while the US average is four times higher at $8,541.(2)
Medicare Advantage
Every fiscal year, CMS updates its MA plan payment policies to reflect changes in risk score trends, coding patterns, and star ratings, among others. For 2023, CMS estimates a positive rate change in net payment impact of 8.5% versus 2022, which should allow MA plans to implement desired strategies to serve beneficiaries while complying with regulatory mandates. Despite the increase, average MA rates on the Island continue to be 41% lower than the average US (PR:$616 Per Member Per Month; US: $1,036 PMPM), also lower than our US Virgin Islands neighbors ($799 PMPM). (3)
Across the United States, we are beginning to see certain trends in Medicare Advantage that are having or will begin to have repercussions on the Island:
- Expansion into new geographies: MA plans are branching out into new landscapes, especially the bigger players. We have seen this materialize in Puerto Rico with the entrance of Elevance (previously Anthem) and GuideWell (a Florida-based Blue Cross Blue Shield plan) with the acquisition of MMM and Triple-S, respectively.
-
Increased focus on Special Needs Plans (SNPs): SNPs are a type of MA plans with tailored benefits and limited enrollment for people with specific diseases. These products demand well-defined Models of Care and the clinical expertise to manage them. The expansion into these types of plans is expected across the US. Puerto Rico-based MA plans already have extensive experience working with special needs populations. There are 313,000 SNP plan enrollees in PR, 6% of all the SNP beneficiaries in the US. Puerto Rico is the fourth jurisdiction in the number of SNP enrollees, only behind Florida, New York, and Texas.(4)
- Plan benefit design focused on Social Determinants of Health (SDoH): Certain MA plans look to target specific populations based on SDoH. For example, Gold Kidney Health Plan in Arizona, a Medicare plan designed for patients with Diabetes, Heart Failure, Cardiovascular Disease, and End-Stage Renal Disease (ESRD); Leon Health, a new MA plan in Miami with a long history of caring for the Cuban population (among others) in their Leon Clinics network; SCAN Health Plan developing an LGBTQ+-focused plan benefits package. This trend of product offerings or condition-specific programs focused on targeted populations is expected to continue in the mainland US. We should see the same trend materializing in Puerto Rico.
Care delivery: Issues continue
Hospitals
Hospitals in Puerto Rico face long-standing financial challenges driven primarily by the funding inequalities mentioned above. Inflation, which peaked at 9.2% in June of 2022, has exacerbated the financial problems of hospitals by increasing operating expenses disproportionately to rates. This is the main issue facing hospital executives in 2023, to the extent that in October, the Hospital Association of Puerto Rico requested the Governor to lobby for $500 million of Medicaid funds to be directed at increasing compensation for clinical workers in hospitals and other health centers.(5)
The hospital sector has seen consolidation in the previous years, and additional moves could materialize in the future. Hospitals or hospital systems with the appropriate capital structure looking to take advantage of economies of scale could acquire less solvent ones.(6)
Physicians
By all accounts, Puerto Rico faces a longstanding crisis of physicians. For many years, better compensation and working conditions in the mainland US have attracted professionals, creating what’s been labeled as a physician exodus on the Island. This phenomenon has extended to Registered Nurses too. In addition to that, physicians on the Island are aging. Data published by the American Medical Association (AMA) show that 47% of active physicians in Puerto Rico are over the age of 60.(7)
Coincidentally, the US sees a shortage in labor supply, with 100,000 nurses and 117,000 doctors leaving their jobs in 2022. Over 40% of doctors and nurses declare they are burnt out. This phenomenon is not unique to the US and Puerto Rico. Around the world, the World Health Organization predicts a shortfall of 15 million healthcare workers by 2030.
Experience: A blueprint for improvement
The patient journeys
In Puerto Rico, patients regularly must wait months to see a doctor when not directly flying outside the island to obtain care. Also, policies and regulations are well-defined but hard to understand from a patient’s standpoint, like pre-authorizations for procedures or specialty medication refills. Payers and providers often struggle to cooperate in productive ways, making it difficult for patients to navigate the system and get the care they need.
Fixing this requires an integrated view anchored in Customer Experience principles and methodology, such as those in V2A’s CX Transformation framework.
First, it is vital to define our promise to the patient clearly. The healthcare promise of “appropriate care by the suitable provider at the right moment” requires communication and unity of purpose among different players, where a shortfall in one instance will impact all others and, ultimately, the patient. At this point, we must understand patient expectations.
Then it is essential to understand the current state of the patient’s journey by mapping the patient’s experience with data and insights, identifying opportunities for improvement, and collaboratively evaluating solutions to improve the journey.
We then must assess whether the organizations involved in fulfilling the defined promise to the patient have the capabilities to do so. Evaluating the internal processes, resources, and systems that interact with the patient will give us improvement opportunities to redesign them. A management infrastructure to manage all the changes needs to be in place, including dashboards with KPIs to monitor the impact on the experience. Lastly, the entire organization must adopt mindsets and behaviors focused on the patient. This often requires embarking on cultural transformations and change management processes.
The health care worker’s journey
Physicians go through a long and tedious bureaucratic process to obtain a valid license to practice Medicine, and often go through hurdles to obtain a contract with a payer to bill for patient care (when not directly denied access to a network), and express frustration when navigating the different payer policies for claims submission and pre-authorization, along with low reimbursement rates for their services.
Nurses and other healthcare workers express concerns over their working conditions and low pay. These issues are at the center of a suboptimal experience for health professionals in Puerto Rico, and we should apply the CX principles outlined above to address them.
An in-depth assessment of their journey may yield improvements that include better credentialing practices, implementing new ways to attract and retain staff (such as flexible scheduling and supportive work culture), a focus on staff engagement and job satisfaction, and the use of AI to support workforce planning and scheduling, thus reducing overworking staff. Please refer to V2A’s insight “The Recipe for a Successful Civil Service Reform” for ideas on how the private sector can implement V2A’s Human Capital Framework to implement these solutions.(8)
Turning vision into action
There is much talk about a vision for patient-centricity and strategies for attracting healthcare workers, but not enough action. We need to turn our good intentions into well-implemented plans with measurable results and accountability baked into them.
Despite funding inequalities with the rest of the jurisdictions in the US and the financial stress many of the providers on the island are going through, there is a big opportunity in front of us. We have the chance to focus on fixing the patient and healthcare workers’ experience of navigating our healthcare system to obtain and provide care.
V2A Consulting will continue to partner with payers, provider groups, non-profits, and government entities to design and implement solutions that improve the healthcare ecosystem. We will continue to put our proven methodologies and Analytic tools along with our market and socio-economic understanding to support these efforts.
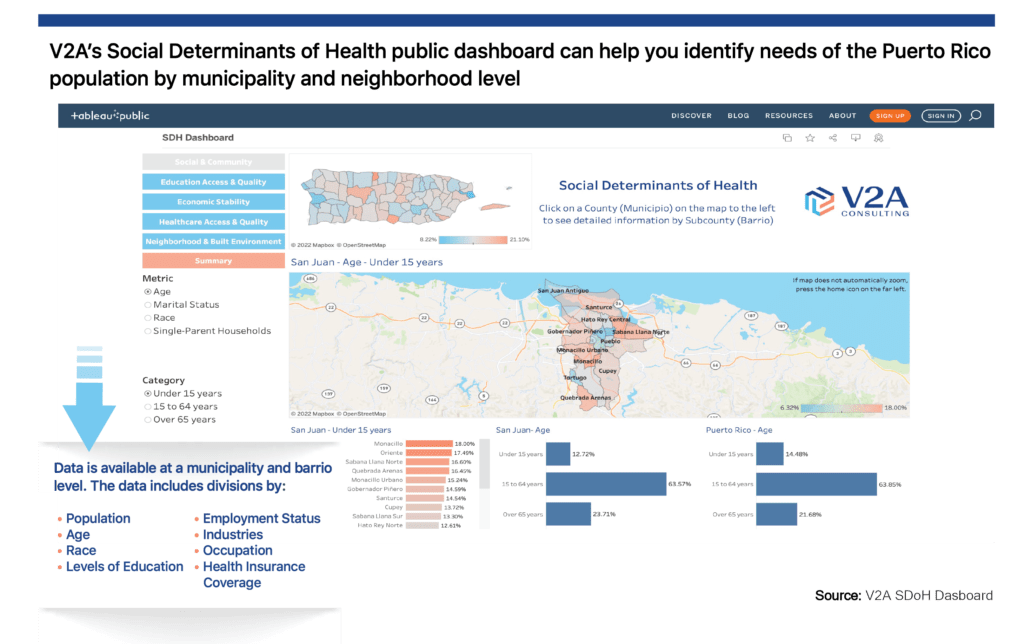
Our SDoH-focused platform provides socio-economic details by community that payers and medical groups can leverage for plan benefit package design and care plan strategies. In addition, non-profits and local governments can better understand the triggers of health outcomes in their communities and devise new funding opportunities to implement programs that address local social and clinical issues while helping to mitigate the funding inequalities in Puerto Rico.
We will continue to use our CX Transformation framework to help every organization define the promise they are making to their patients and healthcare workers and communicate it effectively, including designing customized attraction and retention strategies within an effective human capital framework. We will continue to dive deep, understand each player’s journey, and develop the organizational capabilities in our healthcare organizations that are needed to fulfill those promises.
We aim to continue publishing reports, insights, interviews with sector leaders, and case studies that will enable a productive dialogue around this industry’s issues and, more importantly, reach actionable solutions.
Our reality is challenging. But every sector worker, organization, and the public agency has a vision of a better healthcare system in Puerto Rico.
We’re happy to be in it with you.
For additional information on our Healthcare consulting practice, please visit: https://v2aconsulting.com/healthcare/
For additional inquiries, please email us at: info@v2aconsulting.com
Sources:
(1) ASES Executive Director – https://www.elvocero.com/gobierno/agencias/millonaria-asignaci-n-federal-ayudar-a-frenar-xodo-de-profesionales-de-la-salud/article_914ff4fc-8653-11ed-90d0-8f3aee5189ae.html
(2) 2019 Medicaid data – https://www.medicaid.gov/state-overviews/scorecard/how-much-states-spend-per-medicaid-enrollee/index.html
(3)https://mmapapr.org/wp-content/uploads/2022/04/April-2022-MA-Factsheet-MMAPA-Branded.pdf
(4) CMS December 2022 SNP plans enrollment – https://www.cms.gov/research-statistics-data-and-systemsstatistics-trends-and-reportsmcradvpartdenroldataspecial-needs/snp-comprehensive-report-2022-12
(5) https://www.elvocero.com/actualidad/otros/la-asociaci-n-de-hospitales-pide-500-millones-al-medicaid-para-mejorar-salarios-de-profesionales/article_e95849b8-50b8-11ed-bc69-ebf609fbbff8.html
(6) https://www.elvocero.com/economia/otros/en-estado-cr-tico-la-salud-econ-mica-de-los-hospitales/article_e45f6c18-908f-11ed-8c82-571315e0cf9c.html
(7) American Medical Association (AMA) Physician Masterfile
(8) https://mphdegree.usc.edu/blog/staffing-shortages-in-health-care/
ONLY ENGLISH VERSION
