Summary
- Puerto Rico’s Medicaid Program funding is capped due to its territory status and additional funding approvals are inconsistent and unstandardized.
- Puerto Rico is one of the jurisdictions that spends the least amount of funds per capita when compared to other states due to funding gaps, healthcare infrastructure, and coverage of fewer Medicaid mandatory & optional benefits.
- Puerto Rico is at a disadvantage to meet service access and quality standards required by Medicaid, as the necessary resources are prioritized for delivery of services and not to the transformation of its health system infrastructure.
- The issue must be addressed as almost half of PR’s population get their healthcare coverage through the Medicaid program and are part of indigent population with fewer purchasing power to acquire individual health coverage.
- Current government proposal serves as a band-aid in the short term- as it does not resolve Puerto Rico funding issues and gaps on the long-term. If Puerto Rico returns to current statutory levels, its destined to receive fewer federal transfers contrary to current approved levels.
Introduction
Puerto Rico’s healthcare industry relies heavily on state and federally funded programs, the most important one being Medicaid, locally known as “La Reforma” or “Vital”. Due to the island’s poor socio-economic conditions, the medically indigent community comprises approximately 43 percent of the total population, 56.9 percent when it only comprises children eighteen (18) years or under.[1] However, every so often, the local government struggles to meet the demand for services and finds itself lobbying to receive additional funds through special appropriations. Although the program usually fails to comply with its basic benefit requirements, the Federal Government has remained reluctant to guarantee a recurring stream of funds to meet the island’s Medicaid demands. Throughout this article, we aim to explain and expand on the current state of Puerto Rico’s Medicaid Program funding.
The gap to be bridged
Under federal law, Medicaid funds assigned to Puerto Rico are allocated through a yearly statute, which does not include special appropriations approved by the United States Congress to account for increase in Medicaid funding needs. Usually, these increases in Medicaid funding needs create a funding gap that forces Puerto Rico to request larger amounts each year to cover 1) increases in program beneficiaries and 2) higher utilization rates or service costs.[2] Nonetheless, Puerto Rico would be eligible for a higher share of federal funds to cover this increase in services and eligible population if it were treated as a state. However, Puerto Rico as a territory of the United States has a capped annual allotment[3]which represented $366.7 million dollars in FY2019. This means that regardless of the number of beneficiaries, or any increase in services provided to the island’s indigent community, expected funding appropriations remain untouched. This allotment represented 14 percent of the total appropriated federal funds to cover Medicaid costs in said year.
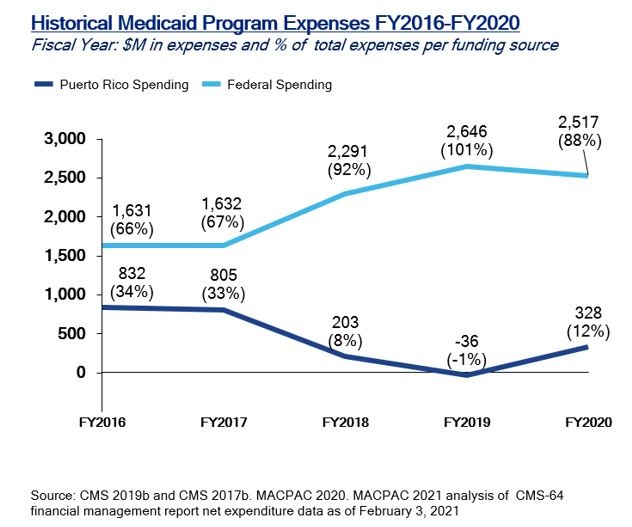
In addition, the Federal Medical Assistance Percentages (FMAP)[5] provides a supplementary statutorily matching scheme which governs the match that the Federal Government provides to cover for each state’s Medicaid expenditures. The matching structure provides automatic adjustments considering demographic and economic shifts, healthcare costs, public health emergencies, and more.[6] In Puerto Rico’s case, its FMAP matching rate is set at 55 percent, whereas if it used the same formula as states, it could receive up to 83 percent.
Notwithstanding the funding caps, programs need to consider funds from an expense perspective to understand the investment scope and effect in mitigating population health needs. Despite the Federal Government’s increase in federal transfers to Puerto Rico for the Medicaid Program, the territory is one of the jurisdictions that spends the least amount of Medicaid funds per capita. Although Puerto Rico lobbying efforts have included efforts to approve recurrent funds linked to population poverty levels, there has been no political climate to consider and approve such proposal. Although Puerto Rico has a lower overall uninsured rate than the United States, its population has a higher prevalence of infant mortality rate and chronic conditions. Due to this, Puerto Rican governments have opted to prioritize approval of additional funds to cover health services associated with this population. For example, the US Department of Health and Human Services reported in a 2017 report that Puerto Rico has a disease prevalence in hypertension of 44.7 percent and diabetes of 17.2 percent. In comparison, the state median for hypertension is 32.3 percent and 10.5 percent for diabetes.[7]
Per Capita Expenditures Compared with Four (4) States with Greatest amount of Hispanic Population
|
Per Capita expenditures estimate for states and territories (2018)[8] |
||||||
| State /
Territory |
Total Population | Children | Adult: non-expansion, under age 65 | Aged (Adults over 65+) | People with disabilities | Adult: ACA Medicaid Expansion |
| Puerto Rico | $ 1,807 | $ 2,108 | $ 2,162 | $726[9] | $ 955 | $2,281 |
| Florida | $ 5,601 | $ 2,072 | $ 2,721 | $14,242 | $ 12,566 | N/A |
| California | $ 6,449 | $ 2,789 | $ 2,812 | $14,548 | $ 23,462 | $5,545 |
| New Mexico | $ 6,381 | $ 3,757 | $ 3,693 | $10,706 | $ 22,184 | $5,637 |
| Texas | $ 9,247 | $ 3,885 | $ 7,108 | $27,168 | $ 27,600 | N/A |
As shown in the table above, Puerto Rico is the jurisdiction with the least amount of spending per capita as compared to States with the highest presence of Hispanic population according to the 2020 Census. Most compelling evidence of this is the fact that Puerto Rico spends 95% less in aged beneficiaries and 93% less in people with disabilities when compared to Florida, the second jurisdiction with the least amount of expenditures.
Under these conditions, Puerto Rico is at a disadvantage to meet service access and quality standards required by Medicaid, together with the necessary resources to transform its infrastructure and mitigate its beneficiary’s health outcomes. Despite the fact that the Puerto Rico Health Insurance Administration (ASES) has integrated some of its data with the Medicaid Management Information System (MMIS), it’s still pending to kick-off Phase 3 of the project related to the development of the Financial Management module of the system. Moreover, the Fiscal Oversight Management Board’s (FOMB) approved Fiscal Plan for Puerto Rico included appropriations towards multiple initiatives aimed to improve its infrastructure. One of them includes the development of a plan to improve clinical operation, data consolidation, and identification of hospital management software solutions.
Currently, Puerto Rico only provides ten (10) (i.e., Physician services, inpatient and outpatient hospital services, etc.) out of the seventeen (17) mandatory benefits required by Medicaid. The Puerto Rico Government has voiced it can only provide these benefits due to current assigned funding and the state of its health infrastructure. Additionally, it offers eight (8) (i.e., dental services, outpatient prescription drugs, physical therapy, etc.) out of the thirteen (13) optional benefits where its availability varies on a state-by-state level. Out of the mandatory benefits, it’s alarming to note that Puerto Rico does not cover 1) home health services, 2) nursing facility services for individuals aged 21 or over, and 3) non-emergency medical transportation (NEMT).[10] Without a doubt, these examples directly impact the recovery process of high-cost high need or ill patients including NEMT. Although Managed Care Organizations (MCO) under the Medicare Advantage Program (MA) have included NEMT as part of its additional benefits, it is only available to certain eligible beneficiaries under MA. Therefore, this results in limited access to care driven in part by lack of transportation, an important social determinant of health.
The level of urgency
In view of this, Puerto Rico remains misaligned with Medicaid’s mission and scope of benefits & services. The endgame is not just the provision of certain health services, but an access to them which directly influence social determinants of health and impact health outcomes. Even though providers are paid less in comparison with states, efforts should not only concentrate on funding expenditure estimates, but on reviewing the elements of our health system to strengthen provider partnerships and deliver better care for program recipients.
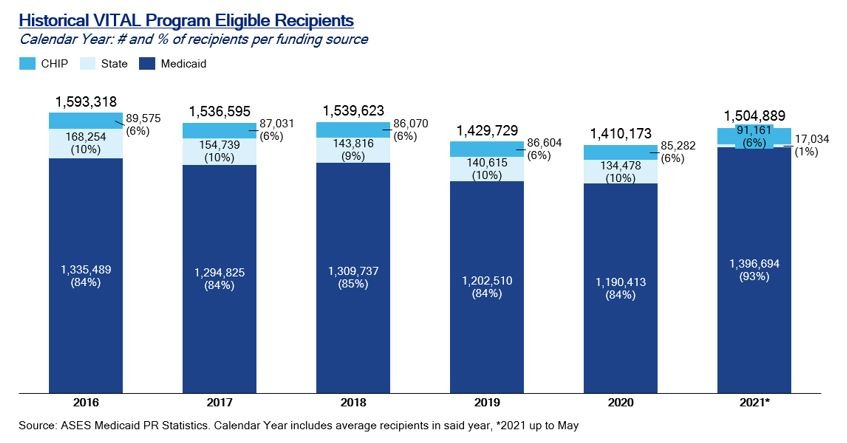
It is important to note the magnitude of this issue since around 1.4 million citizens of Puerto Rico, or roughly 43% of its population, report income lower than the poverty line and almost half of its population receives healthcare coverage through the Medicaid program. Moreover, it’s important to consider Medicaid eligible population has been variable in recent years due to eligibility changes which have been in part driven by the aftermaths of hurricanes, earthquakes, and the pandemic.
The current situation
Although Puerto Rico enjoyed a sigh of relief in 2018 when President Trump signed the Bipartisan Budget Act of 2018, this two-year breather was supposed to come to an end on September 30th when the fiscal year ends, and the island faced an impending Medicaid cliff. Yet, the US Department of Health and Human Services announced on September 15th its interpretation that prior legislation increased the annual Medicaid funding allocation permanently to a new $2.9 billion baseline. This statement aligns to a certain point with President Biden’s proclamation that Puerto Rico should receive equal funding and parity in standing with other states. However, this announcement only pertains to funds allocated via the Social Security Act Section 1108(g) and does not pertain to FMAP matching rate levels and other appropriations. [12]
Every year, Medicaid budget season raises concerns for Puerto Rico’s health officials, but instead of taking action and ending this recurring issue, Congress has opted for a different strategy. Even though President Biden’s budget proposal included equal funding for the Medicaid Program, it did not include a legislative proposal to make such arrangement permanent, and instead called on Congress to legislate on it. Under those circumstances, Congress is in no need to legislate prior to September 30th as the announcement guarantees the $2.9 billion allotment with annual inflation adjustment increases in perpetuity.
The road ahead
All things considered; Congress acted to secure funding in the near short-term outlook but opted for not making this funding permanent and extensive for Puerto Rico. Furthermore, it postponed the discussion of appropriating equal funding in comparison with other States. Yet, the current proposal doesn’t consider system and infrastructure changes needed to provide greater access and quality of care for program recipients. On numerous occasions the Federal Government has called upon Puerto Rico to transform its infrastructure through special technological projects, process optimizations and avoidance of fraud and waste of public funds. An increase in Medicaid expenditures per beneficiary does not entail greater access or services through its manage care programs as it aims to fill gaps and not exceed them.
As of today, legislation includes implementing a set of checks and balances to address concerns from the Federal Government over inferences of misuse of federal funds. Even though such checks and balances could pose short-term obstacles, the program’s stakeholders could benefit from focusing on the underlying long-term challenges that remain unaddressed. A solid partnership between Puerto Rico’s government and the Health Sector is vital to continue supporting ongoing lobbying efforts and provide a long-term solution to these funding gaps as well as allocate resources to renovate the island’s health infrastructure.
V2A’s Healthcare Practice will continue analyzing and developing insights that aim to promote data driven conversations between industry stakeholders and policy makers. The government’s commitment and capacity to generate and publish data will support initiatives to transform this sector and ultimately improve patient’s health outcomes.
Sources and Footnotes
[1] How States Would Fare Under Medicaid Block Grants or Per Capita Caps: Lessons from Puerto Rico, (Commonwealth Fund, Jan 2021) https://doi.org/10.26099/p2s7-4p57
[2] Medicaid an Overview- Congressional Research Service https://crsreports.congress.gov/product/pdf/R/R43357
[3] Total federal Medicaid spending in the territories is subject to an annual Medicaid Cap pursuant to section 1108 of the Social Security Act, Congressional Report from the Office of the Governor of Puerto Rico December 2020 https://medicaid.pr.gov/pdf/Congress/PR%20Response%20to%20PL11694_Requirement%203_Contracting%20Reform%20Plan_Final.pdf
[4]Puerto Rico reports negative territory Medicaid spending due to federal Medicaid spending exceeding total Medicaid spending. Federal spending exceeds total spending due to negative prior period adjustments and the 100 percent FMAP that went into place in FY 2018. Because these prior period adjustments apply to periods. Medicaid and CHIP in Puerto Rico, MACPAC (February 2021)
[5] Federal Medical Assistance Percentages (FMAP): Definition and match rates per States https://aspe.hhs.gov/federal-medical-assistance-percentages-or-federal-financial-participation-state-assistance
[6] How do States Pay for Medicaid? Peter G. Peterson Foundation https://www.pgpf.org/budget-basics/budget-explainer-how-do-states-pay-for-medicaid
[7] Report to Congress on Medicaid and CHIP, June 2020 Chapter 5: Puerto Rico p.78 https://www.macpac.gov/wp-content/uploads/2020/06/June-2020-Report-to-Congress-on-Medicaid-and-CHIP.pdf
[8]Medicaid per Capita Expenditures: Per State and Territories https://www.medicaid.gov/state-overviews/scorecard/how-much-states-spend-per-medicaid-enrollee/index.html
[9] As of August 2021, Puerto Rico has a total of 771K eligible persons for the Medicare program. Out of those, around eighty (80) percent of them are enrolled in a Medicare Advantage (MA) program comparted to mainland United States which is less than half. (Monthly Report by State CMS 08-2021, V2A Analysis)
[10] Report to Congress on Medicaid and CHIP, June 2020 Chapter 5: Puerto Rico https://www.macpac.gov/wp-content/uploads/2020/06/June-2020-Report-to-Congress-on-Medicaid-and-CHIP.pdf
[11] The Children’s Health Insurance Program (CHIP) represents children eligible for health coverage under this program as their family earn too much money to qualify for Medicaid. On the other side, State represents recipients not eligible under Medicaid as they earn too much money, but who are eligible under State criteria and the local government assumes 100% of its costs. However, this group has significantly lowered in recent years with additional funds approved under the Trump Administration but are not considered in future cap levels. https://www.healthcare.gov/medicaid-chip/childrens-health-insurance-program/
[12] White House confirms Medicaid funding for Puerto Rico to avoid a fiscal cliff in the short term https://www.elnuevodia.com/english/news/story/white-house-confirms-medicaid-funding-for-puerto-rico-to-avoid-a-fiscal-cliff-in-the-short-term/
Disclaimer
Accuracy and Currency of Information: Information throughout this “Insight” is obtained from sources which we believe are reliable, but we do not warrant or guarantee the timeliness or accuracy of this information. While the information is considered to be true and correct at the date of publication, changes in circumstances after the time of publication may impact the accuracy of the information. The information may change without notice and V2A is not in any way liable for the accuracy of any information printed and stored, or in any way interpreted and used by a user.
