Puerto Rico is on the brink of a major transformation in how Medicaid reimburses inpatient hospital care. Starting January 1, 2026, all managed care organizations (MCOs) will shift from their current payment models—most commonly per diem, though in some cases capitation, per case, or other structures are used—to the All-Patient Refined Diagnosis Related Group (APR-DRG) classification system for most inpatient claims.
This shift not only responds to the Fiscal Oversight and Management Board’s call for value-based reforms and better cost containment in healthcare but also aligns Puerto Rico with the prevailing U.S. Medicaid standard: more than two-thirds of state Medicaid programs already reimburse inpatient hospital services through DRGs or similar discharge-based systems, with per diem methods increasingly being the exception. In this sense, Puerto Rico is not just complying with an external mandate—it is catching up to a national best practice designed to promote more equitable hospital reimbursement and improve access to care for Plan Vital beneficiaries.
Initially scheduled for October 2020 and subsequently postponed to October 2024 and October 2025, the implementation of APR-DRG has now been rescheduled to January 2026 to provide hospitals and MCOs additional time to adjust their systems and processes. Nevertheless, hospitals were required to purchase and implement the necessary APR-DRG reimbursement software (Solventum is the third-party software vendor used in Puerto Rico) by October 1, 2025, as reaffirmed by ASES Executive Director Carlos Santiago, JD, during the HFMA Puerto Rico Annual Healthcare Update on September 19, 2025.
The change applies exclusively to inpatient services under the Vital program (hospital admissions requiring an overnight stay or longer) and excludes psychiatric hospitalizations, rehabilitation services, long-term care, outpatient surgeries and procedures, as well as urgent care and emergency visits.
What is changing?
APR-DRG vs. current contracting models
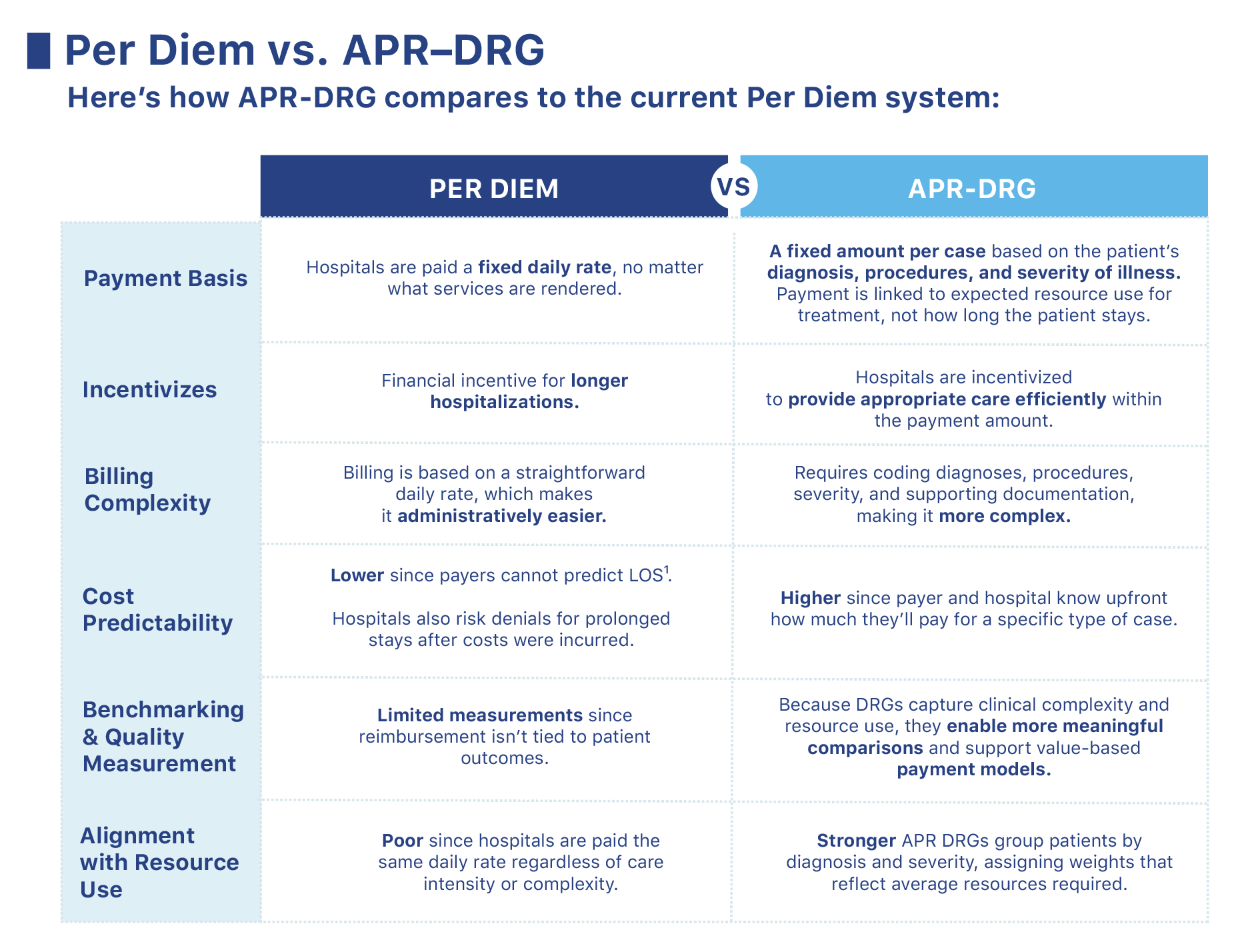
Today, hospitals contract under various operating models including per diem, capitation, per case, or other arrangements. Puerto Rico’s Medicaid program is moving towards a payment model “per case” based on paying diagnostic related groups through the APR-DRG system. Under per diem, the most used model, fees generally increase with length of stay—like a hotel charging per night. However, in practice, extended hospitalizations can result in financial losses, since insurers may deny coverage for additional days, leaving hospitals to absorb the cost. The APR-DRG system instead assigns a fixed payment for each hospital stay based on the type of case and the severity of the patient’s condition, with special adjustments for certain situations.
Think of it as grouping hospitalizations into “buckets,” where each bucket represents patients with similar needs. More complex cases are placed in higher-paying buckets. This approach standardizes reimbursement, making costs more predictable, encouraging efficiency, discouraging unnecessary care, and allowing for fairer comparisons of costs and outcomes across hospitals.
While the transition from Per Diem to APR-DRG represents a significant operational and cultural shift for hospitals, physicians, and payers in the short term, it offers long-term benefits that can improve efficiency, transparency, and fairness across the healthcare system. For hospitals, fixed APR-DRG payments can drive better cost consciousness, improve payment accuracy, and enable the use of data analytics to spot trends and match costs to payments more effectively. For physicians, APR-DRG creates clearer links between clinical documentation, resource allocation, and quality improvement, helping identify performance gaps, support evidence and value -based care, and facilitate meaningful comparisons across patient groups and facilities. Over time, these combined advantages align incentives for efficiency, consistency, and better outcomes—ultimately making the healthcare system more sustainable and equitable for all. Figure 1 below summarizes these key differences to the current Per Diem system.
The Base Rate is the standard dollar amount used in the program design. In Puerto Rico, it is set individually for each hospital based only on paid claims data. Unlike the Medicare DRG system, which relies on hospitals’ actual costs incurred, Puerto Rico’s approach excludes cost reports and unpaid or denied claims. This makes it critical for each hospital to understand its defined base rate and assess how it compares to its true costs, since important cost drivers may not have been contemplated in the current calculation.
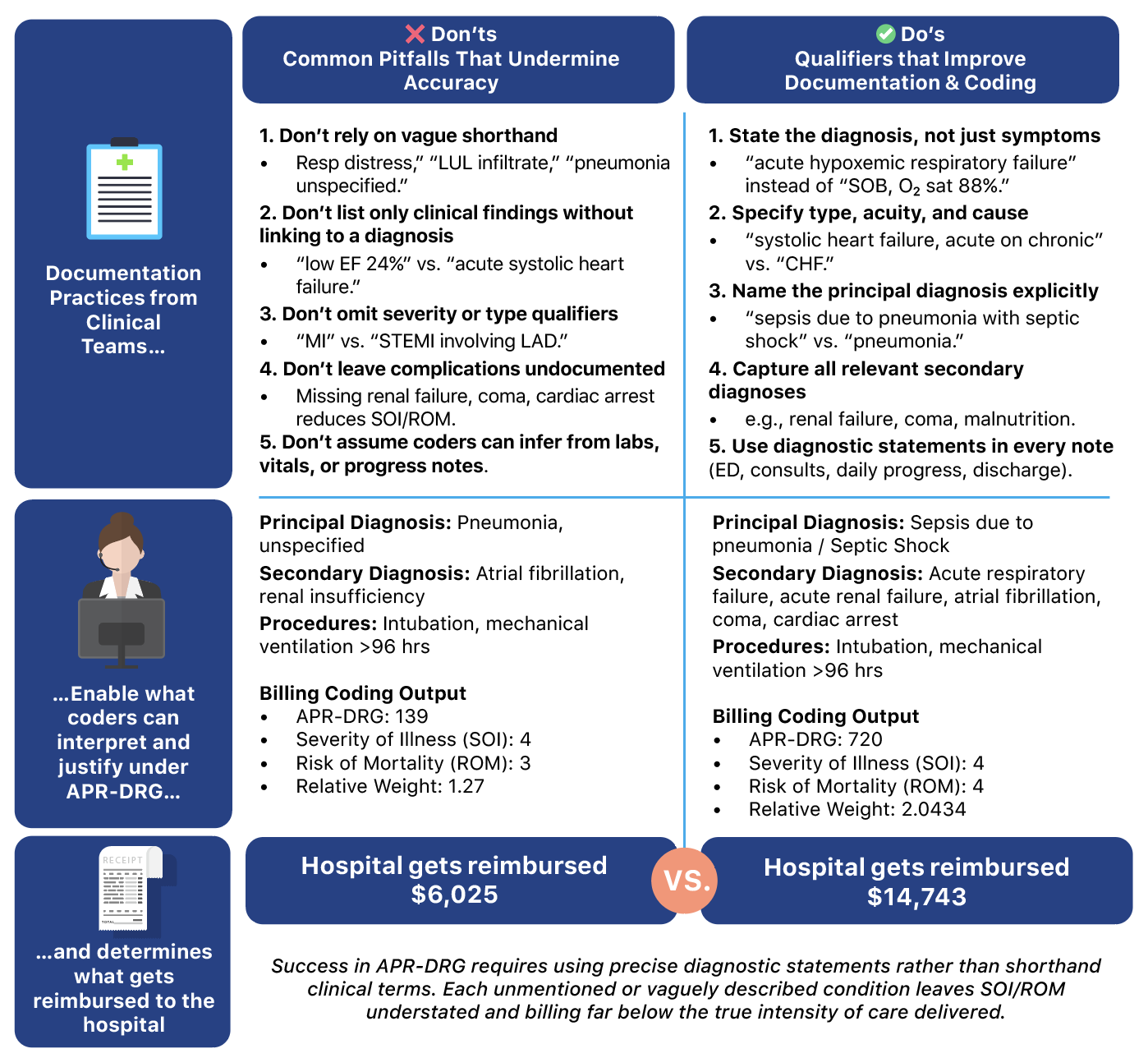
DRG Relative Weights represent the average resources required for a given DRG. They are determined by three key factors: the patient’s reason for admission (DRG), Severity of Illness (SOI), and Risk of Mortality (ROM). Each of these elements must be clearly specified in the claim and fully supported by clinical documentation to ensure hospitals receive the correct payment. This is one of the most critical components to manage accurately, as hospital reimbursement can vary significantly based on the SOI and ROM justifiable within each claim.
Policy Adjusters are options to enhance the base payment for specific providers and/or services, such as trauma providers or high-cost procedures. For Puerto Rico, these are currently not included.
*The formula presented above is the standard payment, it’s important to note that there are other ASES approved payment mechanisms for non-traditional inpatient stays like short stays, transfer of patients from one hospital to another, outlier costs or days.
What does this mean for hospitals?
The transition to APR-DRG in Puerto Rico was designed by ASES, with the support of benefits consulting groups Mercer, to have a budget-neutral impact for hospitals. ASES, with the support of Mercer, reported that the current per diem methodology totals $576 million in inpatient hospital payments for the Plan Vital beneficiaries. Under the approved APR-DRG methodology, it is estimated that this amount will decrease to $516 million; however, a $60 million transition payment pool was established for the first year of implementation to provide hospitals with financial stability as they adapt to the change. It is unknown whether this transition payment pool will continue to be available beyond the first year.
This means hospitals must optimize their processes, teams, and technology to minimize revenue losses—especially after the initial transition period.
During a recent healthcare forum organized by the Colegio de CPA de Puerto Rico, Carmen A. Lliteras, Consulting Director at Galíndez LLC—a local accounting and consulting firm specializing in healthcare and the hospital industry—explained that “the final impact of this transition will ultimately depend on the success of the hospital’s implementation with all teams and how well all areas work together to produce the necessary clinical documentation.”
From admissions to nursing and clinical teams, communication and documentation must be airtight, and electronic records should be thoroughly maintained at every step. Figure 2 below illustrates an clear example of how complete and diagnosis oriented clinical documentation is key for APR-DRG success in hospitals.
The shift to diagnostic statements is a cultural and workflow change.
Success will come from engaging clinicians, reinforcing new habits, and equipping them with tools that simplify accurate documentation at every touchpoint.
Where to Get Started
Checklist for a Successful Transition
1. Understand current financial risk and process gaps
- Obtain and validate your hospital’s base rate information – Request from ASES the hospital’s finalized base rate and, if available, the supporting documentation on how it was calculated. Reconcile this with your own records (noting that ASES used claims data that might not necessarily reflect actual operating cost) and use the Mercer-prepared Excel tool to run test cases under APR-DRG, comparing results with your current payment amounts.
- Project the financial impact on budgets, compliance with covenants, and cash flow. Model and monitor different scenarios based on expected utilization, case mix, and current SOI/ROM documentation levels.
- Identify diagnosis and service lines that will benefit or lose under the new model. Review medical protocols and adjust where reimbursement will not cover costs.
- Consider investments in experienced APR-DRG coders or outsourcing coding during the transition as well as contracting Clinical Documentation Improvement (CDI) specialist’s support or deploying CDI improvement programs to train clinical teams in documenting for APR-DRG. Separately, the transition already requires hospitals to acquire and implement APR-DRG software and ensure its adoption by billing teams.
2. Invest in and focus on successful implementation
- Create an internal implementation team with representation from physicians, nursing, administration, and finance — success depends heavily on clinical team engagement. Studies show that physicians educated on documentation and coding requirements results in more accurate DRG assignments – they need to be in the center of the change.
- Develop a strong change management plan and communicate clearly across the organization: why the change is happening, what is changing, what’s expected from each area, and the risks of not adapting.
- Build a detailed implementation roadmap with governance, accountability, and a cadence for regular progress reviews.
- Monitor not just the completion of tasks, but also early performance metrics and outcomes throughout the first year of implementation. Create transparency mechanisms with operational and clinical teams to maintain momentum, enable accountability, share best practices and course correct along the way.
3. Leverage analytics, digitalization, and AI
- Use data analytics to monitor case mix, SOI/ROM accuracy, denial rates, and revenue trends in real time.
- Integrate APR-DRG software (ASES is using Solventum’s classification system) with your electronic health record (EHR) and financial systems for seamless data flow.
- Implement dashboards for clinicians and administrators to track key documentation and coding performance indicators.
- Explore AI-assisted coding and clinical documentation improvement (CDI) tools to catch missing details, improve accuracy, and flag potential under/over coding before claims go out.
- Adopt OCR (Optical Character Recognition) and NLP (Natural Language Processing) technologies to automatically capture, interpret, and structure data from clinical notes, scanned forms, and other unstructured sources to automate clinical documentation, reducing the administrative burden, and providing consistency and effectiveness for DRG billing purposes.
- Implement ambient listening AI tools that can capture and transcribe provider–patient interactions in real time, creating draft clinical documentation that physicians can review and sign.
- Use NLP algorithms to review clinical documentation completeness and accuracy before claims submission, maximizing the likelihood of optimal payment and reducing denials.
V2A Consulting has the expertise and tools to help hospitals navigate the transition to APR-DRG strategically and effectively minimizing risks while maximizing opportunities. From rethinking your hospital’s strategy, redesigning processes and providing robust project management, to developing and deploying effective change management strategies, and implementing digital, analytics, and AI-driven solutions that optimize coding and documentation, our comprehensive approach ensures every part of your organization is aligned for success. If you would like to discuss how V2A can support your hospital through this change, contact us at info@v2aconsulting.com or reach out to me directly at coralfrederique@v2aconsulting.com to schedule a conversation.
Galíndez LLC is a certified public accounting and consulting firm in Puerto Rico with over 130 professionals, including 44 CPAs. The firm offers services in tax, audit, and accounting, as well as healthcare, management, and IT consulting. As part of the Nexia International network, Galíndez combines local knowledge with access to global resources. For more information, contact info@galindezllc.com.
Sources:
- ASES – Puerto Rico Inpatient Hospital APR-DRGs Hospital Meeting – June 2024
- ASES – Coding for APR-DRGs – October 2024
- ASES – DRG Overview and Hospital Presentation – October 2024
- ASES – Plan Vital FFY26 APR-DRG Hospital Base Rates Version 2 – July 2025
- ASES – Puerto Rico APR-DRG Reimbursement Guide – July 2025
- ASES – Plan Vital APR DRG Live Calculator – July 2025
- Galindez LLC All Patient Refined Diagnosis Related Groups Presentation for the Colegio de CPAs Healthcare Industry Forum – July 2025 (Proprietary presentation – not published – no link)
- Solventum™ All Patient Refined Diagnosis Related Groups (APR DRGs) Classification System | Solventum
 Coral Frederique Guzmán
Coral Frederique Guzmán