The healthcare industry is facing a critical workforce crisis, with burnout driving many health care professionals to leave the field. Excessive workloads, administrative burdens and lack of work-life balance are key contributors to this problem. V2A’s holistic Human Capital Management (HCM) framework can help healthcare organizations address some of these challenges by focusing on optimizing staffing through innovative models, and fostering a patient-centric, supportive workplace culture.
The Challenge
A survey conducted by the American Medical Association (AMA) in 2023 among 12,500 physicians, found that more than one-third (36%) of physicians intend to leave their organization in the next two years.1 Burnout is a widespread problem across various industries, but particularly worrying in healthcare as it leads to mass exit from healthcare professionals which poses access and public health concerns for the wider population. The same AMA survey found that 48% of physicians were experiencing some symptom of burnout. Even though the COVID-19 pandemic exacerbated this burnout, it is not a new phenomenon. Medical professionals have long reported feeling overworked, with a lack of work-life balance triggered by an ever-increasing workload, which coupled with the shortages in labor create a compounding circular effect. The AMA survey also found that 51% of physicians were experiencing a great deal of stress because of their jobs, citing as common stressors: frustrations with the electronic health record (EHR) (33%), lack of adequate staffing (27%) and lack of control over their work schedule (17%).
Puerto Rico has experienced a longstanding physician shortage, with a 2021 study by the Puerto Rico College of Physicians and Surgeons indicating that the island had lost approximately 15,000 doctors over the previous decade, leaving only around 9,000 active physicians to serve a population of over 3.2 million people.3 This physician exodus is largely driven by less competitive compensation, administrative burdens, and the lure of better opportunities in the mainland United States.
A recent Puerto Rico Healthcare Workforce Study commissioned by the Federal Oversight and Management Board and conducted by FTI Consulting 4 sheds some light on the current situation of burnout on the island among healthcare professionals in general, including physicians, nurses and allied health professionals such as therapists and technicians. “After experiencing the 2017 hurricanes, the 2019 earthquakes, the COVID-19 pandemic, and ongoing challenges in healthcare and Puerto Rico more broadly, most stakeholders interviewed and surveyed agreed that the healthcare workforce in Puerto Rico is experiencing severe burnout”. Poor working conditions as seen in Figure 1, coupled with heavy workloads because of healthcare professional shortages, contribute to ongoing chronic burnout.


Of special concern is the experience of Nurses, whose burnout rates are excessively high, with 92% of them always, mostly and sometimes feeling burnout as seen in Figure 2. These rates surpass those in the mainland U.S, where feeling of burnout among Nurses has gone down from 90 percent in 2021 to 81 percent in 2023. Nurses tend to spend more time on administrative tasks compared to physicians and less time focused on patient care. The study found that 63% of nurses are seeking additional income and only 42% plan to remain in healthcare. Many nurses are leaving Puerto Rico to mainland US healthcare facilities where the wages are two to three times higher.
For all types of healthcare workers, insufficient compensation is the biggest problem faced. Nevertheless, there are other factors that significantly contribute to burnout as seen in Figure 3.

This situation presents urgent public health concerns as the island’s healthcare system is under significant strain, with staffing shortages leading to longer patient wait times, reduced access to specialists, and increased pressure on the remaining workforce. Addressing these systemic issues, as well as the administrative challenges, is critical to safeguarding both healthcare professionals' well-being and the population’s health outcomes. We recognize that given the financial challenges in healthcare that the island faces, improving compensation and benefits might not be a feasible short-term fix. Nevertheless, there are other factors that can be addressed to improve healthcare professional attraction and retention on the island.
The Approach
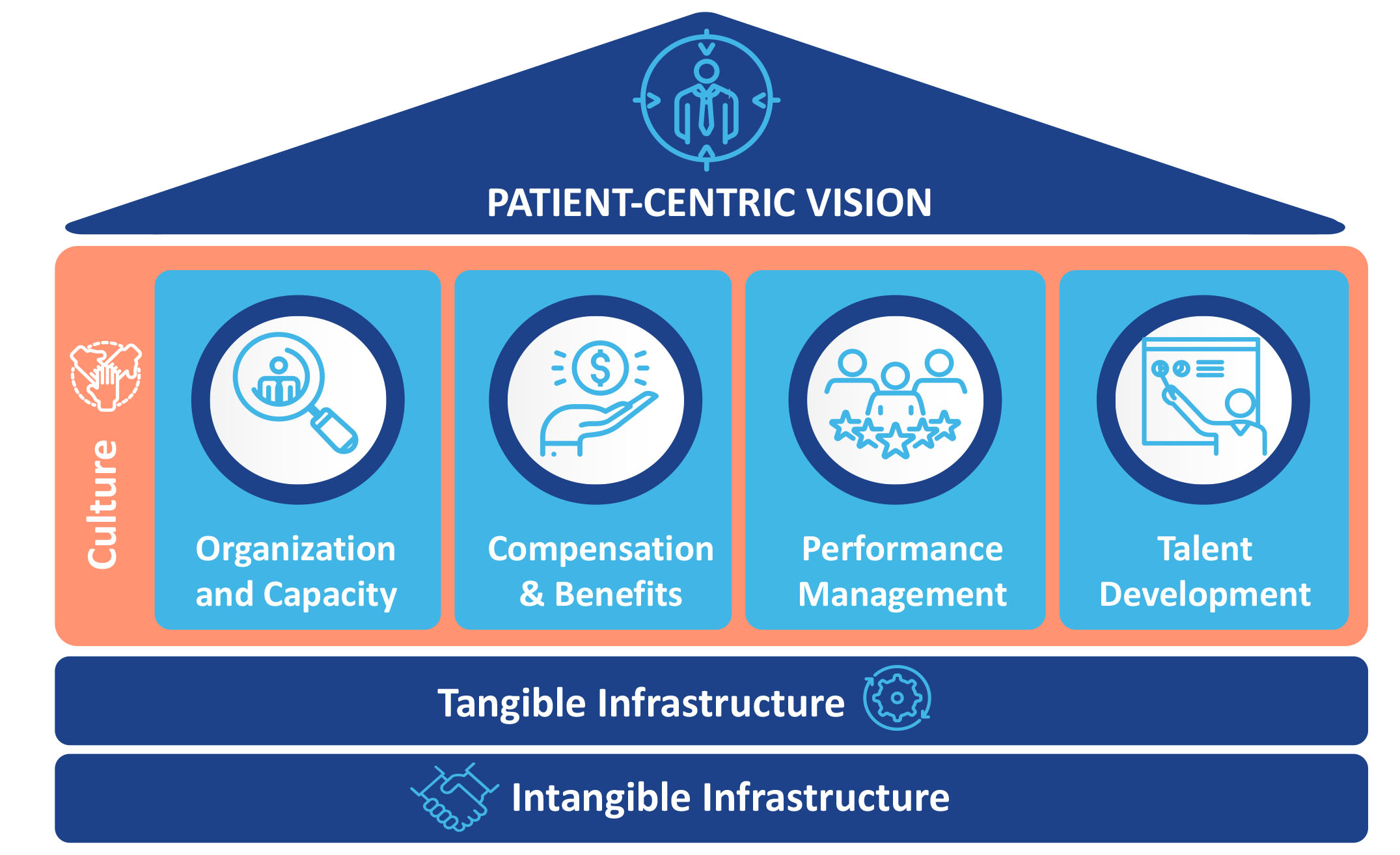
V2A’s Human Capital Strategy framework can help empower organizational leaders to look beyond surface level issues and define specific, achievable goals to attract and retain healthcare professionals in this complicated context.

Now more than ever, investing in innovative technologies is essential to improving clinician experience and patient outcomes. Emerging tools automate administrative tasks, simplify documentation, and enhance care coordination. AI-powered assistants and voice recognition streamline note-taking, while integrated platforms unify patient records and billing. These solutions reduce time spent on non-clinical work, enabling providers to focus on care. By adopting such technologies, healthcare organizations can combat burnout, increase efficiency, and strengthen their appeal as employers in a competitive market.






Conclusion
Considering the recent exit of health care professionals both in the US and in Puerto Rico, hospitals must thoughtfully consider strategies to attract and retain talent, and to address burnout. Healthcare professionals are the center of our healthcare system, and they directly shape patients’ outcomes and experience. In a landscape where personnel are scarce, hospitals must distinguish themselves as great places to work. Through V2A’s Human Capital Management framework, we can help healthcare organizations evaluate and implement the strategies that best fit their vision and budget. Measuring the effectiveness of these strategies and interventions will also be critical in identifying and adopting sustainable solutions. By investing in and supporting your most valuable asset, your people, high-quality patient care is secured now and in the future.
To begin, healthcare organizations can ask themselves: How can I improve my employee’s ability to center the patient experience? Will my current plans support the attraction and retention of health care professionals? Do I understand my organization’s culture and are there any gaps between the current and desired state that can be addressed? Asking these and other questions will allow leaders to evaluate the direction of their organization and its human capital strategy.
Ready to transform your organization? Contact us at gracielasalcedo@v2aconsulting.com or visit www.v2aconsulting.com/contactus to speak with one of our experts.
Authors: Graciela Salcedo, Coral Frederique
Collaborators: Beatriz Delgado
References:
- Findings from the American Medical Association Organizational Well-Being Survey, 2023
- Puerto Rico Healthcare Workforce Study, Feb. 2025, FTI Consulting
- Colegio de Médicos Cirujanos de Puerto Rico. (2021). Physician Workforce Data. Retrieved from https://www.cmcpr.org/
- Puerto Rico Healthcare Workforce Study, Feb. 2025, FTI Consulting
- Puerto Rico Healthcare Workforce Study, Feb. 2025, FTI Consulting
- Addressing Health Worker Burnout (hhs.gov)
 Graciela Salcedo
Graciela Salcedo Coral Frederique Guzmán
Coral Frederique Guzmán

